How COVID-19 vaccines developed in less than a year
| Date :09-Dec-2020 |

WASHINGTON :
HOW could scientists race out COVID-19 vaccines so fast without cutting corners? A head start helped -- over a decade of behind-the-scenes research that had new vaccine technology poised for a challenge just as the coronavirus erupted. “The speed is a reflection of years of work that went before,” Dr Anthony Fauci, the top US infectious disease expert, told ‘The Associated Press’. “That’s what the public has to understand.” Creating vaccines and having results from rigorous studies less than a year after the world discovered a never-before-seen disease is incredible, cutting years off normal development. But the two US front-runners are made in a way that promises speedier development may become norm -- especially if they prove to work long-term as well as early testing suggests. “Abject giddiness,” is how Dr. C Buddy Creech, a Vanderbilt University vaccine expert, described scientists’ reactions when separate studies showed the two candidates were about 95 per cent effective.
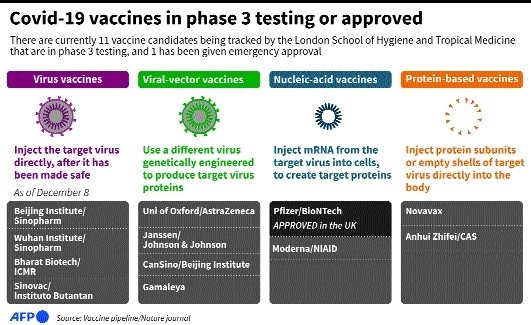
“I think we enter into a golden age of vaccinology by having these types of new technologies,” Creech said at a briefing of the Infectious Diseases Society of America. Both shots -- one made by Pfizer and BioNTech, the other by Moderna and the National Institutes of Health -- are so-called messenger RNA, or mRNA, vaccines, a brand-new technology. US regulators are set to decide this month whether to allow emergency use, paving the way for rationed shots that will start with health workers and nursing home residents. Billions in company and Government funding certainly sped up vaccine development — and the unfortunately huge number of infections meant scientists didn’t have to wait long to learn the shots appeared to be working.
But long before COVID-19 was on the radar, the groundwork was laid in large part by two different streams of research, one at the NIH and the other at the University of Pennsylvania — and because scientists had learned a bit about other coronaviruses from prior SARS and MERS outbreaks. “When the pandemic started, we were on a strong footing both in terms of the science” and experience handling mRNA, said Dr Tal Zaks, chief medical officer of Massachusetts-based Moderna. Traditionally, making vaccines required growing viruses or pieces of viruses — often in giant vats of cells or, like most flu shots, in chicken eggs — and then purifying them before next steps in brewing shots. The mRNA approach is radically different.
It starts with a snippet of genetic code that carries instructions for making proteins. Pick the right virus protein to target, and the body turns into a mini vaccine factory. “Instead of growing up a virus in a 50,000-liter drum and inactivating it, we could deliver RNA and our bodies make the protein, which starts the immune response,” said Penn’s Dr. Drew Weissman.